·临床研究·
安小虎, 徐 韬, 王 苑, 柴 静, 徐子锋
(上海交通大学医学院附属国际和平妇幼保健院麻醉科,上海 200030)
【摘要】目的 评价右美托咪定复合曲马多用于剖宫产术后镇痛的效果。方法 择期行剖宫产产妇150例,数字随机表法随机分为3组: Ⅰ组于胎儿取出后静脉注射生理盐水20ml,术后静脉自控镇痛(PCIA)药物配方为曲马多1g,生理盐水稀释至100ml,设置背景输注剂量为1.5ml/h,PCA 2ml,锁定时间15min;Ⅱ组于胎儿取出后静脉注射右美托咪定0.3μg/kg,生理盐水稀释至20ml,微泵10min静脉推注完毕,术后PCIA配方和设置同Ⅰ组。Ⅲ组于胎儿取出后静脉微泵推注右美托咪定0.3μg/kg,使用方法同Ⅱ组,术后PCIA配方为曲马多1g+右美托咪定200μg,生理盐水稀释至100ml,术后PCIA设置同Ⅰ组。观察术后4、8、24h VAS评分、Ramsay镇静评分和曲马多的用量;观察术后6h恶露排除量和泌乳开始时间;记录24h内心动过缓、低氧血症、恶心、呕吐、眩晕等并发症的发生情况和产妇对术后镇痛的满意度。结果 3组产妇一般情况无统计学意义,均完成了24h镇痛观察,没有产妇需要额外的镇痛治疗。与Ⅰ、Ⅱ组比较,Ⅲ组术后4、8、24h VAS评分和曲马多用量降低,产妇满意度提高(P<0.05);三组产妇术后6h恶露排出量,产后泌乳开始(挤压双侧乳房有明显乳汁泌出)时间无统计学意义;三组产妇术后各时间点Ramsay评分有所不同,但无统计学意义,术后均未发生心动过缓、低氧血症、恶心呕吐等副作用,Ⅰ组、Ⅱ组、Ⅲ组各有5、1、0例产妇术后第一次起床时出现眩晕症,未特殊处理,休息后好转。结论 右美托咪定复合曲马多用于择期剖宫产术后静脉镇痛效果优于单独使用曲马多。
【关键词】右美托咪定; 曲马多; 剖宫产术; 镇痛; 产妇控制
右美托咪定是高选择性α-2肾上腺素能受体激动剂,具有镇静、镇痛、抗焦虑等作用,且没有明显呼吸抑制作用[1]。研究表明,术后镇痛复合使用右美托咪定可以降低阿片类药物用量[3-4]。曲马多属于弱阿片受体激动剂,主要通过抑制5-羟色胺和去甲肾上腺素的吸收,减少神经冲动的传递而发挥镇痛作用,作为静脉镇痛药由于乳汁中含量少而在剖宫产术后的镇痛中受到广泛青睐,但单独使用容易出现恶心呕吐和眩晕等副作用。理论上两药物合用有协同镇痛效果,可能较单一曲马多镇痛减少其用量,本研究拟评价右美托咪定复合曲马多用于剖宫产术后镇痛的效果,为临床运用提供参考。
1.1 一般资料
择期行剖宫产产妇150例,年龄24~41岁,身高156~171cm,孕周37+5~40+2周,体质量65~88kg。无产科高危因素和内科相关合并症,无长期使用镇痛、抗焦虑或其他精神病类药物的病史。本研究经医院伦理委员会批准,产妇和家属签署有知情同意书。
1.2 分组情况
择期行剖宫产产妇150例,数字随机表法随机分为3组: Ⅰ组于胎儿取出后静脉注射生理盐水20ml,术后静脉自控镇痛(PCIA)药物配方为曲马多(批号: H20091073,德国格兰泰有限公司)1g,生理盐水稀释至100ml,设置背景输注剂量1.5ml/h,PCA 2ml,锁定时间15min;Ⅱ组于胎儿取出后静脉注射右美托咪定(批号: H20090248,江苏恒瑞医药股份有限公司)0.3μg/kg,生理盐水稀释至 20ml,微泵10min静脉推注完毕,术后PCIA配方和设置同Ⅰ组。Ⅲ组于胎儿取出后静脉微泵推注右美托咪定0.3μg/kg,使用方法同Ⅱ组,术后PCIA配方为曲马多1g+右美托咪定200μg,生理盐水稀释至100ml,术后PCIA设置同Ⅰ组。
1.3 麻醉方法
所有产妇均无术前用药,入室后开放静脉,输注乳酸林格氏液,监测HR、BP、SPO2和EKG。产妇均采用右侧卧位,定位于L3~4/L2~3间隙,利用针内针法行蛛网膜下腔穿刺,待脑脊液自然流出后注入0.5%罗哌卡因11~13mg,向头端置入硬膜外导管4cm并固定后翻身,手术床左倾15°,观察麻醉平面至T6后开始手术。手术开始后不再椎管内使用局麻药、静脉内不用任何镇静和镇痛药物,术中持续鼻吸氧,当收缩压低于90mmHg或产妇有低血压相关恶心呕吐、胸闷等主诉时,静脉注射麻黄碱10~30mg。手术结束时按分组情况进行相关治疗,后接静脉镇痛泵(Automed 3300韩国)行静脉自控镇痛。
1.4 观察项目
分别于术后4、8、24h随访和记录产妇VAS评分(0为无痛,10为最痛)、Ramsay镇静评分和曲马多的用量;观察术后6h产妇恶露排除量,记录产后泌乳开始(挤压双侧乳房有明显乳汁泌出)时间;随访术后24h产妇对镇痛的满意程度(非常满意、满意、一般、不满意);记录24h内心动过缓(心率<60次/min)、低氧血症(SpO2<90%)恶心、呕吐、眩晕等并发症的发生情况。
1.5 统计学处理
采用SPSS 13.0统计学软件进行分析,正态分布的计量资料以![]() 表示,组间比较采用方差分析,组内比较采用重复测量设计的方差分析,其他计量资料和等级资料比较采用秩和检验,P<0.05为差异有统计学意义。
表示,组间比较采用方差分析,组内比较采用重复测量设计的方差分析,其他计量资料和等级资料比较采用秩和检验,P<0.05为差异有统计学意义。
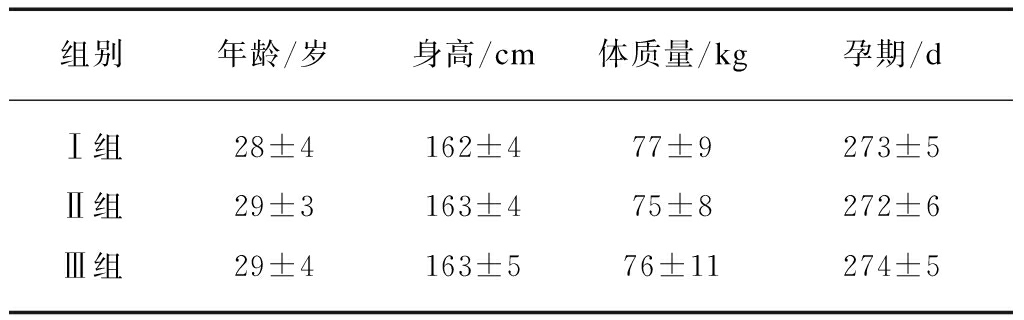
三组产妇一般资料比较无统计学意义(P>0.05),见表1。
表1 三组产妇一般资料比较
Tab.1 Comparison of maternal general information in 3 groups![]()
三组产妇均完成了24h镇痛观察,没有产妇需要额外的镇痛辅助治疗。
与Ⅰ、Ⅱ组比较,Ⅲ组产妇术后4、8、24h VAS评分和曲马多用量降低,产妇满意度提高(P<0.05);见表2、3。
表2 三组产妇VAS评分和曲马多用量比较
Tab.2 The VAS scores and tramadol dosage comparison in three groups![]()

注: *与组Ⅰ比较,P<0.05;#与组Ⅱ比较,p<0.05
表3 三组产妇满意度比较
Tab.3 Comparison of maternal analgesia satisfaction in three groups (n)
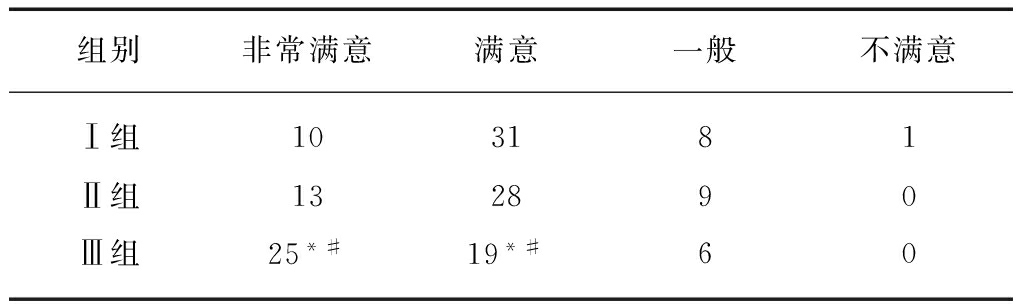
注: *与组Ⅰ比较,P<0.05;#与组Ⅱ比较,P<0.05
三组产妇术后6h恶露排出量,产后泌乳开始时间无统计学意义。
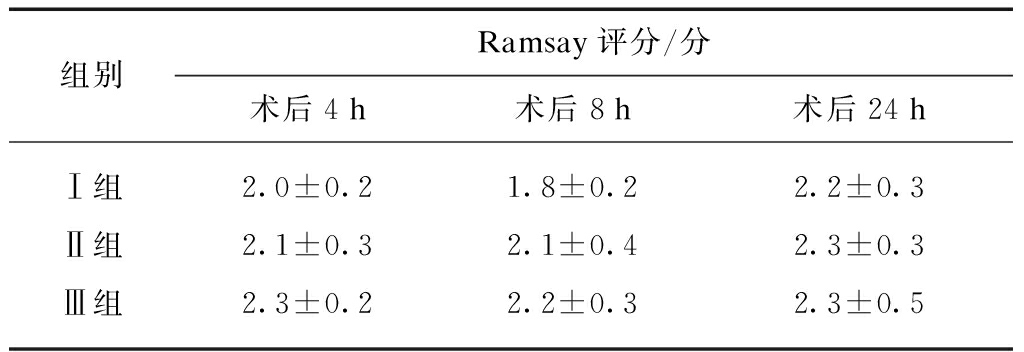
和Ⅰ、Ⅱ组比较,Ⅲ组产妇术后4、8时间点Ramsay评分有显著性差异,见表4。
三组产妇各时段均未发生心动过缓、低氧血症、恶心呕吐等副作用,Ⅰ、Ⅱ、Ⅲ组各有5、1、0例产妇术后第一次起床时出现眩晕症,未特殊处理,休息后好转。
表4 三组产妇各时间点Ramsay评分
Tab.4 Ramsay scores of three groups at different time points
右美托咪定是高选择性α-2肾上腺素能受体激动剂,具有镇静、镇痛、抗焦虑等作用,且没有明显呼吸抑制作用[1-3]。研究表明,术后镇痛复合使用右美托咪定可以降低阿片类药物用量[4-6]。曲马多属于弱阿片受体激动剂,主要通过抑制5-羟色胺和去甲肾上腺素的吸收[7],减少神经冲动的传递而发挥镇痛作用,作为静脉镇痛药由于乳汁中含量少而在剖宫产术后的镇痛中受到广泛青睐。
本研究结果显示三组产妇均完成了镇痛观察,没有产妇需要额外的镇痛治疗,镇痛效果满意。和Ⅰ、Ⅱ组比较,Ⅲ组非常满意和满意的产妇比例有显著提高,说明右美托咪定和曲马多联合使用的效果优于曲马多单独使用,4、8、24h产妇VAS评分和和曲马多用量减少,印证了这一结论。Ⅱ组和Ⅰ组比较,镇痛效果差异不显著,说明单纯0.3μg/kg的负荷剂量偏小,尚达不到镇痛的效果。
三组产妇的镇静评分无显著差异,说明右美托咪定复合曲马多静脉镇痛,不影响产妇的镇静程度。三组泌乳开始时间、6h内的恶露排除量无显著差异,提示右美托咪定不影响泌乳时间,也对产后子宫收缩无影响。三组产妇心动过缓、恶心呕吐等副作用无显著差异,说明右美托咪定不增加镇痛的副作用。三组产妇中各有5、1、0产妇在第一次起床时出现眩晕,可能与曲马多的副作用有关,右美托咪定是否具有预防或治疗曲马多导致的眩晕尚不能得出结论,有待进一步大样本量的观察。
本研究结果提示,右美托咪定复合曲马多用于择期剖宫产术后静脉镇痛效果优于单独使用曲马多。
【参考文献】
[1] Ebert TJ, Hall JE, Barney JA, et al. The effect of increasing plasma concentrations of dexmedetomidine in humans[J].Anesthesiology,2000,93: 382-394.
[2] Stemp LI, Karras GE JR. Dexmedetomidine facilitates withdrawal of ventilatory support[J].Anesthesiology,2006,104(4): 890.
[3] Angst MS, Ramaswamy B, Davies MF, et al. Comparative analgesic and mental effects of increasing plasma concentrations of dexmedetomidine and alfentanil in humans[J].Anesthesiology,2004,101(3): 744- 752.
[4] Palanisamy A, Klickovich RJ, Ramsay M, et al. Intravenous dexmedetomidine as an adjunct for labor analgesia and cesarean delivery anesthesia in a parturient with a tethered spinal cord.Int J[J].Obstet Anesth,2009,18(3): 258-261.
[5] Yuyan N, Yuqi L, Qingyan L, et al. Effect of dexmedtomidine combined with sufentanil for post-caesarean section intravenous analgesia[J]. Eur J Anaesthesiol,2014,31: 197-203.
[6] Lin TF, Yeh YC, Lin FS, et al. Effect of combining dexmedetomidine and morphine for intravenous patient-controlled analgesia[J]. Br J Anesth,2009,102(1): 117-122.
[7] Akbay BK, Yildizbas S, Gualu E, et al. Analgesic efficacy of topical tramadol in the control in the of posyoperative pain in children after tonsillectomy[J].J Anesth,2010,24: 705-708.
Efficacy of dexmedetomidine combined with tramadol for patient-controlled intravenous analgesia after cesarean section
AN Xiao-hu, XU Tao, WANG Yuan, CHAI Jing, XU Zi-fen
(Dept. of Anesthesiology, International Peace Maternal and Obstetrical Hospital, Shanghai Jiaotong University, Shanghai 200030, China)
【Abstract】Objective To evaluate the efficacy of dexmedetomidine combined with tramadol for patient-controlled intravenous analgesia (PCIA) after cesarean section. Methods One hundred and fifty patients undergoing elective cesarean section were randomly allocated into 3 groups with 50 cases in each group. Immediately after delivery, a bolus of dexmedetomidine 0.3μg/kg was given intravenously in 10 min in groupⅡand group Ⅲ, while normal saline (NS) was given in groupⅠinstead. GroupⅠand group Ⅱ received PCIA with tramadol 1g diluted by NS into 100ml (background infusion 2ml/h; PCA 2ml; lockout interval 15min); group Ⅲ received PCIA with dexmedetomidine 200μg combined with tramadol 1g diluted by NS into 100ml (background infusion 2ml/h; PCA 2ml; lockout interval 15min). VAS scores, Ramsay scores and consumption of tramadol were measured 4, 8 and 24h after surgery. The volume of lochia 6h after surgery and the time of breast milk secretion were recorded. The side effects like bradycardia, hypoxemia, nausea, vomiting and dizzy 24h after surgery were also recorded. The degree of satisfaction of post-operative analgesia was documented. Results There were no statistical differences in patients demographics among three groups, and no patient needed extra analgesia. The VAS scores and the consumption of tramadol of 4, 8 and 24h were lower and the degree of satisfaction was higher in group Ⅲ than those in groupⅠand group Ⅱ(allP<0.05). There were no statistical differences in volume of lochia and the time of milk secretion among 3 groups. Ramsay scores were 2 at all time points in thee groups. No side effects like bradycardia, hypoxemia, nausea, vomiting and dizzy were observed after surgery. Conclusion Dexmedetomidine combined with tramadol offers better analgesic effect than single use of tramadol after cesarean section.
【Key words】Dexmedetomidine; Tramadol; cesarean section; analgesia; patient control
doi:10.16118/j.1008-0392.2016.03.016
收稿日期:2016-02-29
作者简介:安小虎(1965—),男,副主任医师,学士.E-mail: tigeran173@aliyun.com.cn
通信作者:徐 韬.E-mail: 18918098660@163.com
【中图分类号】R 719.8
【文献标志码】A
【文章编号】1008-0392(2016)03-0080-04